Does UV Light Actually Disinfect and Kill Viruses?
By Shannon Bauer
Before you start waving a handheld wand over every nook and cranny in your home, find out what experts have to say about UV light’s disinfection abilities, including whether or not it can kill coronavirus.
After months of frantic hand washing, social distancing, and mask-wearing, it seems that the coronavirus has dug its claws in for the long haul in the U.S. And since the few parts of this scary experience you can control are your own actions and environment, it’s no wonder that you — and practically everyone else — have become cleaning-obsessed. If you didn’t stock up on Clorox and disinfectant wipes back in March, you’ve likely become a pro at navigating Google to find answers to questions such as “can steam kill viruses?” or “is vinegar a disinfectant?” Your missions down the research rabbit hole might’ve even led you to other novel ways of killing germs: namely, ultraviolet (UV) light.
UV light has been used for decades (yes, decades!) to reduce the spread of bacteria, such as that which causes tuberculosis, according to the U.S. Food and Drug Administration (FDA). As for its ability to kill COVID-19 germs? Well, that’s not so well-established. Keep reading to find out the expert-backed truth about UV light, including whether or not it can actually prevent coronavirus transmission and what to know about the UV light products (i.e. lamps, wands, etc.) you’ve seen all over social media.
But first, what is UV light?
UV light is a type of electromagnetic radiation that’s transmitted in waves or particles at varying wavelengths and frequencies, which make up the electromagnetic (EM) spectrum, says Jim Malley, Ph.D., a professor of civil and environmental engineering at the University of New Hampshire. The most common type of UV radiation? The sun, which produces three different types of rays: UVA, UVB, and UVC, according to the FDA. Most people are familiar with UVA and UVB rays because they’re to blame for sunburns and skin cancer. (Related: Ultraviolet Radiation Causes Skin Damage — Even When You’re Indoors)
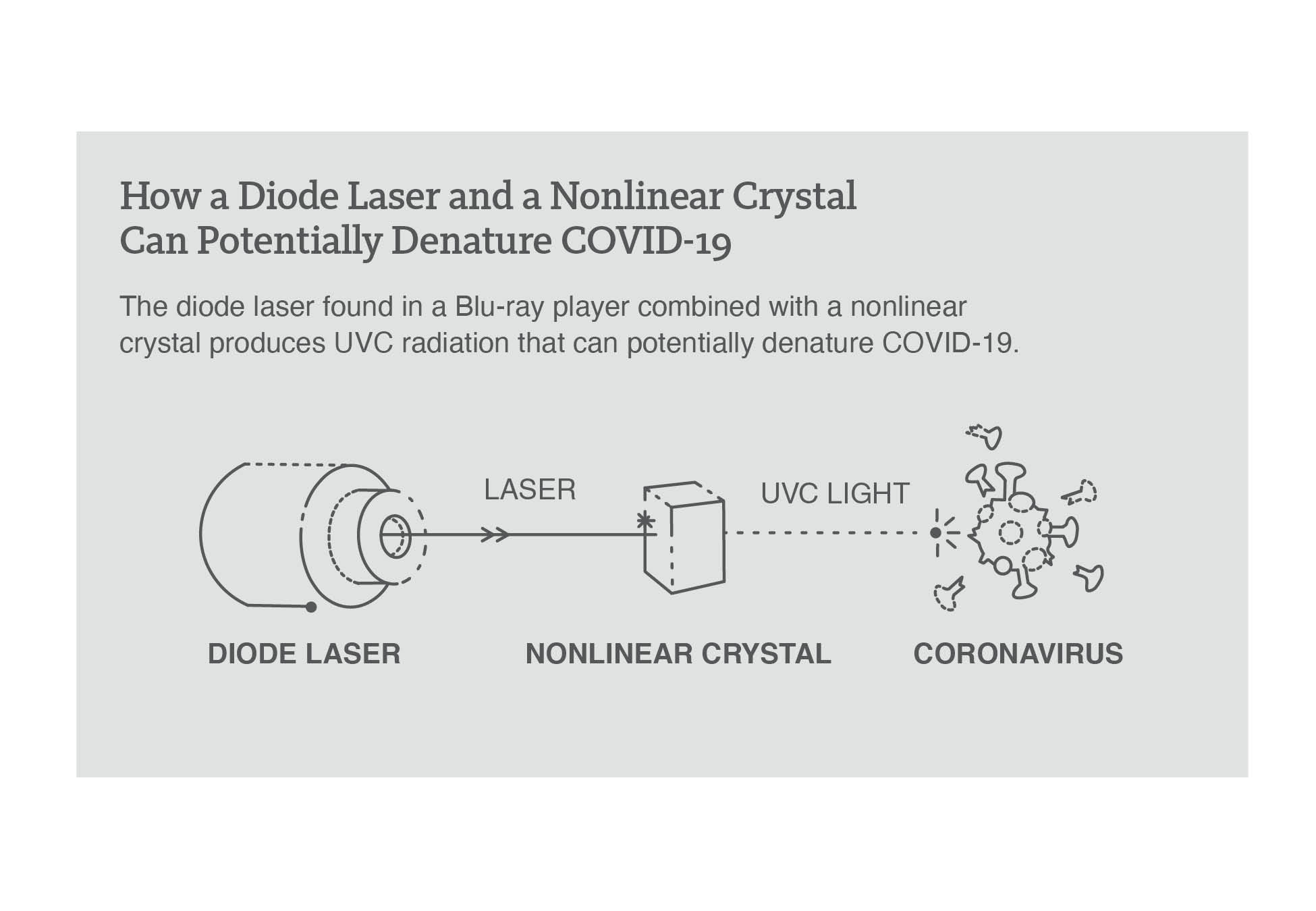
UVC rays, on the other hand, never actually make it to the Earth’s surface (the ozone layer blocks ’em), so the only UVC light humans are exposed to is artificial, according to the FDA. Still, it’s pretty damn impressive; UVC, which has the shortest wavelength and the highest energy of all the UV radiation, is a known disinfectant for air, water, and nonporous surfaces. So, when talking about UV light disinfection, the focus is on UVC, says Malley. Here’s why: when emitted at certain wavelengths and for specific amounts of time, UVC light can damage the genetic material — DNA or RNA — in bacteria and viruses, inhibiting their ability to replicate and, in turn, causing their normal cellular functions to break down, explains Chris Olson, microbiologist and program manager of Infection Prevention and Emergency Preparedness at UCHealth Highlands Ranch Hospital. (Note: While UVC rays from artificial sources can also pose risks including burns of the eye and skin — similar to UVA and UVB rays — the FDA upholds that these injuries “usually resolve within a week” and that the chance of developing skin cancer “is very low.”)
It’s also essential that the area is free of anything that could interfere with the UVC light getting to the target, says Malley. “We refer to UV disinfection as a line-of-sight technology, so if anything blocks the UV light including dirt, stains, anything casting shadows then those ‘shaded or protected’ areas will not be disinfected.”
If that sounds a bit complex, that’s because it is: “UV disinfection is not simple; it’s not one size fits all,” emphasizes Malley. And that’s just one reason why experts and research are still unsure exactly how effective, if at all, it can be against the coronavirus. (See also: How to Keep Your Home Clean and Healthy If You’re Self-Quarantined Because of Coronavirus)
Can UV light disinfection be used against COVID-19?
UVC has a track record of being very effective against SARS-CoV-1 and MERS, which are close relatives of SARS-CoV-2, the virus that causes COVID-19. Several studies, including reports cited by the FDA, have found that UVC light may have the same effectiveness against SARS-CoV-2, but many have not been extensively peer-reviewed. Plus, there’s limited published data about the wavelength, dose, and duration of UVC radiation required to inactivate the SARS-CoV-2 virus, according to the FDA. Meaning more research is needed before anyone can officially — and safely — recommend UVC light as a trusted method for killing coronavirus.
That being said, UV lamps have been and continue to be widely used as a means of sterilization within, for example, the healthcare system. One such reason? Research has found that UVC rays can cut transmission of major superbugs (such as staph) by 30 percent. Many (if not most) hospitals use a UVC-emitting robot that’s about the size of a dorm room refrigerator to sterilize entire rooms, says Chris Barty, a physicist and distinguished professor of physics and astronomy at the University of California, Irvine. Once people leave the room, the device gets to work emitting UV rays, self-adjusting to the size of the room and variables (i.e. shadows, hard-to-reach places) to administer the light for as long as it deems necessary. This could 4-5 minutes for smaller rooms such as bathrooms or 15-25 minutes for larger rooms, according to Tru-D, one type of this device. (FWIW, this is done in tandem with manual cleaning using EPA-approved disinfectants.)
Some medical facilities also use UVC cabinets with doors to disinfect smaller items such as iPads, phones, and stethoscopes. Others have actually installed UVC devices in their air ducts to disinfect recirculated air, says Olson — and, given the fact that COVID-19 spreads primarily through aerosol particles, this set-up makes sense. However, these medical-grade devices are not intended for individual use; not only are they prohibitively expensive, costing upward of $100k, but they also require proper training for effective operation, adds Malley.
But if you’ve spent ample time researching COVID-19 disinfectants, you know that there are at-home UV gadgets and gizmos hitting the market at warp speed right now, all of which purport sanitizing potential from the comfort of your home. (Related: The 9 Best Natural Cleaning Products, According to Experts)
Should you buy UV light disinfection products?
“Most home UV light disinfection devices that we have examined and tested [through our research at the University of New Hampshire] do not achieve the levels of germ-killing that they claim in their advertisements,” says Malley. “Most are under-powered, poorly designed, and might claim to kill 99.9 percent of germs, but when we test them they often achieve less than a 50 percent kill of germs.” (Related: 12 Places Germs Like to Grow That You Probably Need to Clean RN)
Barty agrees, saying that the devices do in fact emit UVC, but “not enough to really do anything in the amount of time claimed.” Remember, for UV light to really kill germs, it needs to be shining for a certain period of time and at a certain wavelength — and, when it comes to effectively killing COVID-19, both of these measurements are still TBD, according to the FDA.
While experts are unsure of the effectiveness of UV disinfection devices against coronavirus, especially for at-home use, there’s no denying that, pre-pandemic, UVC light had been shown (and even used) to kill other pathogens. So, if you want to give, say, a UV lamp a try, it’s quite possible that it’ll help slow the spread of other germs hiding in your home. A few things to keep in mind before you buy:
Mercury is a no-no. “Hospitals often use mercury vapor-based lamps because they can make a lot of UVC light and disinfect in a relatively short time,” says Barty. But, ICYDK, mercury is toxic. So, these types of UV lamps require extra caution during cleaning and disposal, according to the FDA. What’s more, mercury lamps also produce UVA and UVB, which can be dangerous for your skin. Look for mercury-free devices, such as Casetify’s UV sanitizer (Buy It, $120 $100, casetify.com) or those that are labeled “excimer-based,” meaning they use a different method (sans-mercury) to deliver UV light.
Pay attention to wavelength. Not all UVC products are created equal — especially when it comes to wavelengths. As mentioned earlier, the UVC wavelength can impact a device’s effectiveness at inactivating a virus (and thus killing it). It may also impact the health and safety risks associated with using the device, leaving you with the challenge of finding a UV light disinfection device that’s powerful enough to kill pathogens without presenting too much of a health risk. So what is the magic number? Anywhere between 240-280 nm, according to the Centers for Disease Control and Prevention (CDC). That being said, a 2017 study found that wavelengths ranging from 207-222 nm can also be effective and safe (although, not as easy to come by, according to the International Commission on Non-Ionizing Radiation Protection). TL;DR — if it gives you peace of mind or comfort to kill even a few germs on your phone, go for gadgets that emit, at most, 280 nm.
Consider your surface. UVC light is most effective on hard, non-porous objects, according to the FDA. And tends to be ineffective on surfaces with bumps or ridges, as these make it hard for the UV light to reach all the places where the virus might reside, explains Barty. So, disinfecting a phone or desktop screen might be more productive than, say, your rug. And if you really want to wave around a UV light sanitizing wand (Buy It, $119, amazon.com) as if it’s a lightsaber, your best bet is to do so over, for example, your kitchen countertop (think: smooth, nonporous, germy).
Choose products that close. A wand-like UV device isn’t your best bet, says Malley. “Living tissues (humans, pets, plants) should not be routinely exposed to UVC light unless it’s in a carefully controlled setting with well-trained and experienced medical professionals,” he explains. That’s because UVC radiation can potentially cause eye injuries (such as photophotokeratitis, essentially a sunburned eye) and skins burns, according to the FDA. So instead exposed light products like a wand or lamp, opt for “enclosed devices” that come with “safety features (automatic shut off switches, etc.) the eliminate the potential to expose living tissues to stray UVC light,” says Malley. One good option: “A container for your phone, especially if [your phone is] left in there for a long time (while sleeping),” such as PhoneSoap’s Smartphone UV Sanitizer (Buy It, $80, phonesoap.com).
Don’t look into the light. Since the long-term effect of UVC on humans is unknown, it’s important to be extremely cautious while using a device. Avoid continued contact with the skin and steer clear of staring straight at the illumination, as direct exposure to UVC radiation may cause painful eye injuries or burn-like skin reactions, according to the FDA. But, ICYMI earlier, the UV disinfection devices you can buy off the ‘gram or Amazon are, in Malley’s words, “underpowered” and come with automatic shut-off features, limiting risks. Still, better to be careful, considering we don’t fully understand the risks. (Related: Could Blue Light from Screen Time Be Damaging Your Skin?)
Bottom line: “Look for a product with a well prepared and thorough user’s manual, clear specifications of what the UV device delivers for dose, and some evidence of independent third-party testing to confirm the performance claims being made by the product,” suggests Malley.
And until there’s more research and concrete findings that UVC light can in fact kill COVID-19, it’s likely best to just stick to cleaning on the reg with CDC-approved products, stay diligent with social distancing, and, please wear that mask.
Read full article on Shape.com.